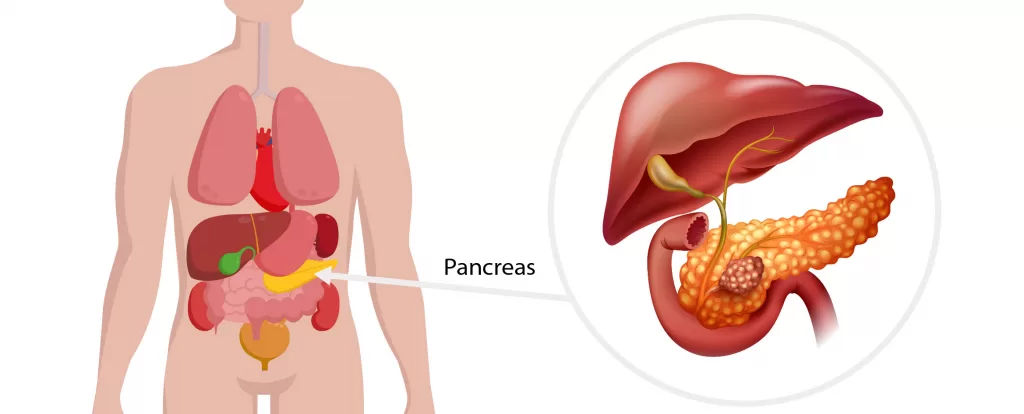
Pancreatic surgery (Pancreatectomy/ Pancreatic resection) is usually undertaken for cancer of the pancreas or related structures (e.g. bile duct cancer). It can also be undertaken for pre-cancerous conditions of the pancreas or rarely for patients with inflammatory (non-cancerous) conditions such as chronic pancreatitis.
Surgery and chemotherapy together offer the only realistic chance to cure pancreatic cancer, which is often associated with poor survival depending on the subtype and stage of cancer.
Surgery of the pancreas is complex and recovery for patients can be a prolonged process. Although most people are in hospital for about a week, hospital stay can be longer in the event of complications and a full recovery outside of hospital can take weeks to months. The team at Harbour Surgery Centre are here to support you every step of the way.
Your surgeon at Harbour Surgery Centre will discuss what type of surgery is right for you if surgery is required. This will depend on many factors including where the cancer is in the pancreas and how much of the pancreas is affected.
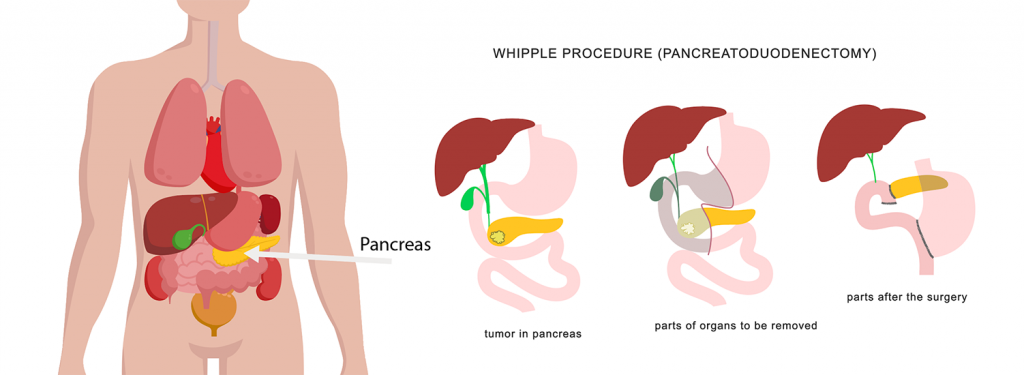
WHIPPLE PROCEDURE (PANCREATICODUODENECTOMY)
The Whipple procedure (named after Allen Oldfather Whipple) is an operation to remove lesions (usually cancers) confined to the head or neck of the pancreas.
The surgeon will remove the head of the pancreas. They also remove:
- the lower end of the stomach
- the duodenum (first part of the small intestine)
- the gall bladder (which stores a fluid called bile that helps digestion)
- part of the bile duct (which carries bile from the liver to the duodenum)
- surrounding lymph nodes (part of the immune system).
Such extensive surgery is necessary often to remove the cancer entirely and also because these organs share blood supply. The remaining bile duct and pancreas are then attached to the small intestine so that bile and digestive enzymes can still go into the small intestine. The end pieces of the small intestine (or the stomach and small intestine) are then reattached so that food can pass through the digestive tract (gut).
DISTAL PANCREATECTOMY
A distal pancreatectomy involves removal of the body and tail of the pancreas. The spleen is also often removed due to shared blood supply and associated lymph nodes. The spleen helps your body fight infections, so if it’s removed, you will need vaccinations before and after surgery to help lower the risk of getting particular kinds of infections. Your surgeon at Harbour Surgery will help coordinate this all for you.
TOTAL PANCREATECTOMY
A total pancreatectomy removes the whole pancreas, the duodenum, the gall bladder, part of the bile duct and sometimes part of the stomach and the spleen. You may have a total pancreatectomy if there is a large tumour, more than one tumour, or if the remaining pancreas isn’t healthy.
It’s possible to live without a pancreas. But when the entire pancreas is removed, people are left without the cells that make insulin and other hormones that help maintain safe blood sugar levels. As a result, patients may develop diabetes and need insulin. People who have had this surgery also need to take pancreatic enzyme pills to help them digest certain foods. Before you have this operation, your surgeon will recommend that you get certain vaccines because the spleen will be removed.
Pancreatic surgery is complex and requires a team with a lot of skill and experience. It carries a risk of complications, some of which can be life threatening. The team at Harbour Surgery perform these operations routinely both in Private practice and in Public.
Even though pancreatic surgery is safe, patients can have complications from the surgery. These can include:
- Leaking from the various connections between organs that the surgeon has to join
- Infections
- Bleeding
- Trouble with the stomach emptying after eating
- Trouble digesting some foods (which might require taking some pills to help with digestion)
- Weight loss
- Changes in bowel habits
- Diabetes
After surgery, patients are managed in a monitored facility before transferring to the ward. Oral intake is introduced slowly and your surgeon will keep a close eye on your progress after surgery with careful clinical examination and investigations such as blood tests. Most patients are in hospital for about a week.