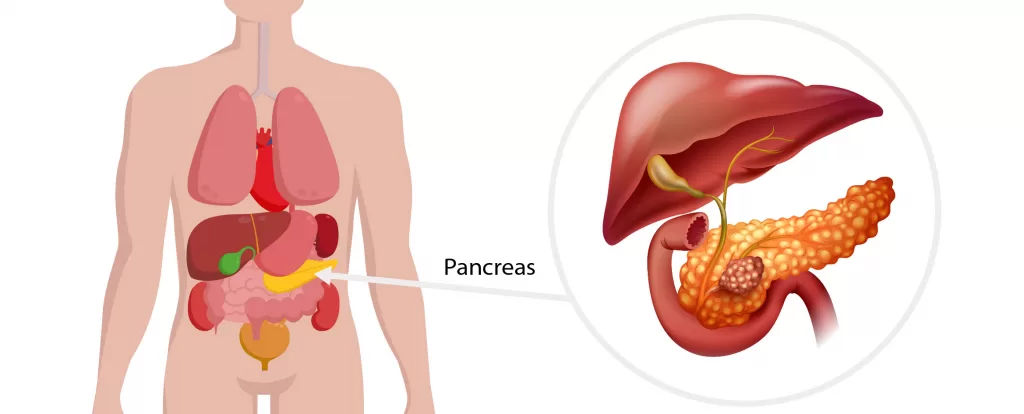
Pancreatic lesions often present as a mass detected on imaging (CT scan and occasionally ultrasound scans undertaken to investigate abdominal symptoms such as pain, indigestion, jaundice or nausea.All pancreatic masses need to be formally investigated and a diagnosis established, most commonly with CT scan, MRI scan, PET scan or endoscopic biopsy.
Many pancreatic masses are benign and non-cancerous. Localised swelling can occur in part or all of the pancreas due to inflammation (pancreatitis) caused by gallstones, alcohol or some medications.
Additionally, masses can form within the pancreas during foetal development with small collections of normal splenic tissue (ectopic spleen) or fat (intrapancreatic lipoma), and intrapancreatic lymph nodes not uncommonly seen.
Most commonly pancreatic masses are divided into cysts (masses that contain fluid usually saline or mucous) or solid benign tumours that do not contain fluid.
Benign tumours of the pancreas are uncommon and usually arise from the pancreatic cells that secrete hormones like insulin. These are usually diagnosed by their appearance on CT or MRI scan and occasionally by direct biopsy.
The need to treat benign pancreatic soft tissue masses is tailored to the diagnosis. All symptomatic masses (either because of their size or due to the effects of hormone secretion) are removed. Small (2 cm or less in diameter) lesions are often observed with CT or MRI scans over several years since the risk of symptoms or development of later cancer at this size is extremely low.
Polyps of 7mm or greater in size are observed annually with ultrasound and those 10mm in size or greater we recommend laparoscopic cholecystectomy to treat and allow the polyp to be examined by a pathologist.
Occasionally surgery is recommended for smaller polyps particularly if they are causing symptoms (eg pain) or they are associated with gallstones. Both of these factors have been shown to increase the risk of cancer in associated with gallbladder polyps.