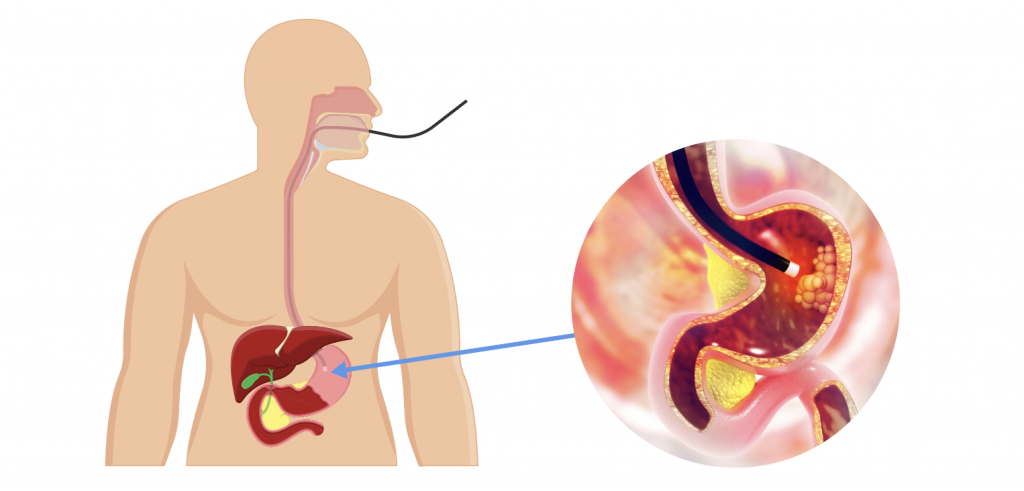
Endoscopy is a medical procedure that allows a doctor to examine the inside of the body using a flexible tube with a tiny camera attached to the end of it. The tube, called an endoscope, is inserted into the body through a natural opening, such as the mouth, nose, or anus, or through a small incision. Endoscopy is a semi-invasive procedure. An Upper GI Endoscopy (Gastroscopy) is when a fibre-optic telescope is inserted under sedation from the mouth to look at the mouth, the oesophagus, the stomach and part of the small intestine. A colonoscopy is when a fibreoptic telescope is introduced under sedation from the anus to look at the anus, rectum, entire colon and the last part of the small intestine.
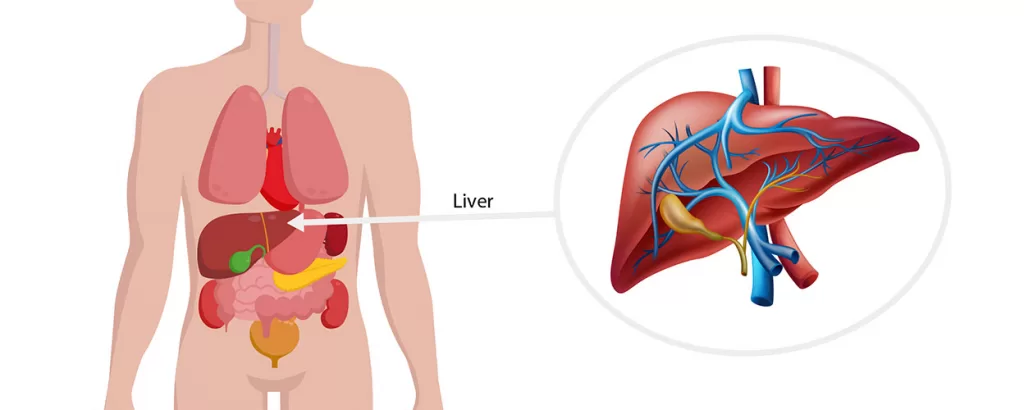
As the endoscope is moved through the body, the camera sends images to a monitor, allowing the doctor to see and assess the condition of organs, tissues, and structures inside the body. Depending on the type of endoscopy, the doctor may also be able to take samples of tissue for further examination, or perform certain medical treatments through the endoscope. Sometimes, just looking via endoscopy is enough to make a diagnosis (for example-a hiatus hernia). Biopsies can also be taken during endoscopy to help diagnose a problem and in select circumstances, treatment can be accomplished such as resection of an early stomach cancer.
Endoscopy is commonly used to diagnose and treat conditions of the digestive tract, such as ulcers, inflammation, and cancers. Your specialist can discuss the role of endoscopy in your care both from a diagnostic and therapeutic perspective.